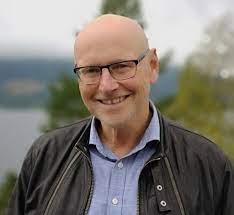
Ole Andreas Underland
Psychiatric nurse, healthcare entrepreneur, and pioneer of the world’s first medication
free psychiatric hospital
Areas of interest
- Reimagining Mental Health care
- Hiking and Fitness
- SAINT-EMILION Bordeaux Wine
Ole Andreas is a psychiatric nurse and healthcare entrepreneur from Norway – with more than 40 years experience working in the psychiatric system, often with clients who have not responded to a traditional treatment approach.
Ole Andreas believes that the psychiatric health care system must change our approach to mental health challenges dramatically. He believes we must stop categorising people into those that are sick, and those that are healthy and instead put energy into helping people lives their best lives with whatever health challenges they have.
Ole Andreas Underland is the founder and Director of the Hurdalsjøen Recovery Centre in Norway which provides “medication-free” care. The private hospital is located about forty minutes north of Oslo, on the banks of stunning Lake Hurdal and was set up to provide “medication-free” care and support to safely taper from psychiatric drugs. It is currently closed, due to a change in public funding, but has plans to reopen. The hospital operated successfully, with no safety or quality issues, for 8 years, had 60 patients across two hospital sites, and operated at full capacity for the final three years until it was forced to pause operations. The Centre still operates recovery communities, and a housing offering, but the hospitals are currently closed until new funding arrangements are agreed. It truly was a revolution, and the first in the world of its kind, as Ole describes in an interview with Robert Whitaker:
“In 2010, patient organisations succeeded in persuading the parliament that there should be treatment alternatives in Norway and it should be a part of Norwegian psychiatry – so patients could choose a medication free
alternative care pathway, or to taper from their psychiatric medication. But by 2013 such a place still didn’t exist. The leader of a well known patients’ organisation in Norway, called the White Eagle,
(Jan-Magne Sorensen) asked me to help. It was clear to me that if we were going to create a recovery-oriented hospital, half of the staff should have lived experience.
Then, one year later, I was asked by another large psychiatric hospital if I could help them with five very chronically ill psychiatric patients who had been hospitalised for 10 to 15 years, and if I could help them get out of the hospital.
As a principle, we have not taken private-paying patients. We have always been 100% publicly financed – which is why we are currently having to pause our service. That’s also a statement we took because what we have been doing is to make [our hospital] part of the public system of Norway so that there would be no discussion about profit and earning money.
In all ways, our hospital is an ordinary psychiatric hospital within the framework of the Norwegian legal system and healthcare system. We have had the same numbers of nurses, psychiatrists, and psychologists, and followed the same rules, but offered a recovery-oriented medication-free treatment programme. I think we are the first in the world to attempt such a model.
The treatment consists of three pillars. IMR—Illness Management and Recovery Therapy – happens five days a week, one and a half to two hours every day, except on the weekends.
Then it’s the high-intensity training, five days a week. We do high-intensity training, because it is important for our heart health.
Food is also central. We have the best restaurant in the north of Oslo, with excellent chefs. We cater for all kinds of diets, but within an environment that is therapeutic – clean air, a nice view, a forest, lake, and the most important thing, good people with the right attitude. And of course, half of the staff have lived experience and understand how to live with difficult states of mind, and how to deal with it too.
We have had 800 patients over 8 years. 80%-90% of the people who chose our service were patients who had previously tried mainstream psychiatry and most of them have had very tragic experiences. Many of them have been traumatised by forced treatment, especially by forced medication. And that’s why we avoided forced treatment and restrictive practices.
We had government approval for forced treatment, and a bed for fixation [restraint], which is something you have to have when you have patients on forced treatment, but it has never been used. We decided to get this approval so patients on forced treatment orders from other hospitals could come to our hospital.
In eight years, we never had a single complaint about the use of forced treatment. That was the main argument for medication-free treatment by the users organisations. If we will get rid of forced treatment, and engage people in activities and structure with good food and access to fresh air and opportunities, we give people something they can believe in and an alternative to medication.”
Abridged from an interview on Mad in America.