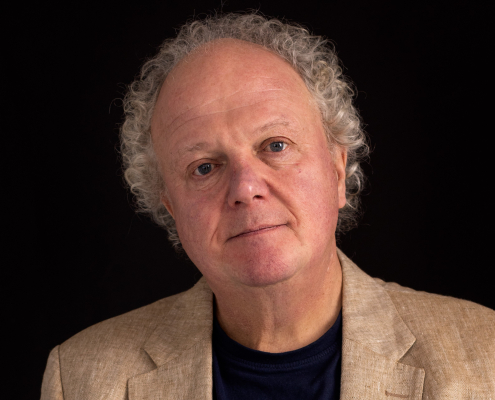
Catherine Thorley
Catherine is Clinical lead for Open Dialogue at the North East London NHS Foundation Trust – one of the research trial sites comparing Peer Supported Open Dialogue (POD) with treatment as usual.
Areas of interest
- Open Dialogue
- Eye Movement Desensitisation and Reprocessing (EMDR)
Cathy is Clinical lead for Open Dialogue at the North East London NHS Foundation Trust (NELFT) – one of the research trial sites comparing Peer Supported Open Dialogue (POD) with treatment as usual.
Cathy is a Systemic Family Psychotherapist and Association of Family Therapy (AFT) approved supervisor, and former NELFT Dialogue First Manager. She completed a two year international trainers training in Open Dialogue in Helsinki in 2018, and is also a tutor on a four week residential POD training leading to a post graduate certificate in Open Dialogue from London South Bank University. Cathy also completed Systemic Leadership Training at The Tavistock in 2016.
Cathy has set up and managed a non-crisis NHS Open Dialogue style service which takes referrals nationally and works with others to support the POD trial at NELFT. She is passionate about working dialogically with families and teams and has found Open Dialogue to be life changing both personally and professionally.
Cathy is also an Eye Movement Desensitization and Reprocessing Therapy (EMDR) consultant – an integrative psychotherapy approach for the treatment of trauma.
Open Dialogue
Open Dialogue is a compassionate approach that involves working with the whole family or network, rather than just the individual, and equipping staff of all disciplines with the key skills to do this, and thus effect change at deeper levels.
The Open Dialogue approach is both a philosophical/theoretical approach to people experiencing a mental health crisis and their families/networks, and a system of care, developed in Western Lapland in Finland over the last 25-30 years.
In the 1980s psychiatric services in Western Lapland were in a poor state, in fact they had one of the worst incidences of the diagnosis of schizophrenia’ in Europe. Now they have the best documented outcomes in the Western World. For example, around 75% of those experiencing psychosis have returned to work or study within 2 years and only around 20% are still taking antipsychotic medication at 2 year follow-up.
Remarkably, Open Dialogue is not an alternative to standard psychiatric services, it is the psychiatric service in Western Lapland. This has afforded a unique opportunity to develop a comprehensive approach with well-integrated inpatient and outpatient services. Working with families and social networks, as much as possible in their own homes, Open Dialogue teams work to help those involved in a crisis situation to be together and to engage in dialogue.
It has been their experience that if the family/team can bear the extreme emotion in a crisis situation, and tolerate the uncertainty, in time shared meaning usually emerges and healing/recovery is possible. Open Dialogue has drawn on a number of theoretical models, including systemic family therapy, dialogical theory and social constructionism.
Open Dialogue has been taken up in a number of countries around the world, including much of the rest of Scandinavia, Germany and several states in America.