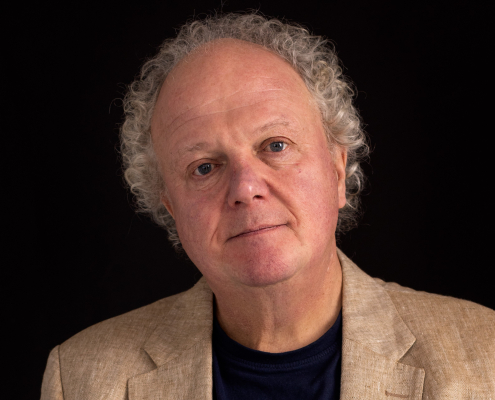
Ciara Glynn
Peer worker in north Dublin and an occasional lecturer delivering peer support, lived experience & recovery education.
Areas of interest
- Depathologising distress
- Reimagining Mental Health care
- Rights based, recovery-orientated approach
Ciara is a peer support worker in north Dublin and an occasional lecturer delivering peer support, lived experience & recovery education. She also facilitates/develops courses with the Dublin North, North East Recovery College, and believes in depathologising human distress and normalising emotional challenges. She’s been working in the Irish Mental health service (HSE) for seven years in a community mental health team, and is also the lived experience representative at Kyrie Farm and a board member at Mental Health Reform. She says:
“One part is the work that I do with people and that’s really based on building a connection. I have my own experience of living with distress and recovery, and access to services. So I use all that experience in my role to be just there for people. So that’s one part of the role and then I see the other part of the role is really an advocacy piece.
The peer support history comes from a very activist and radicalised history of people standing up and wanting change in their services. I would be very vocal on the team about, you know, changing into more recovery-oriented practices, trauma – informed care and rights-based approaches
Can you speak a little bit about the importance of listening to the voice of people with lived experience in the mental health sector?
For me, it’s very important that we listen to the voice of the people with lived experience because historically the voice of the people with lived experience was shunned in services and in traditional practices of how we viewed and helped people who had mental health challenges.
Then I think for many years their voice wasn’t listened to and that’s why there were so many people I suppose harmed and let down by services. I mean, the lived experience piece to me, it’s knowledge, and it’s expertise in itself.
Unless you’ve received a letter in the door which said you were referred to psychiatric service, unless you left the house terrified having to go to an appointment, unless you’ve sat in a waiting area for hours waiting on a doctor, unless you’ve experienced involuntary admission, you know, unless you’ve really experienced any of those things, and you can have empathy, of course, so many people do, but you really, really don’t understand it.
So for me all of those things are knowledge. There’s power in all of that knowledge that services should really be honoring and acknowledging that that is a knowledge base in itself. We should bring in the lived experience voice to the forefront of everything we do, it’s of great importance.
What would you consider to be the most pressing or one of the most pressing issues in mental health in Ireland today?
I suppose for me, the overarching issue that encompasses all the issues is the need for a paradigm shift away from the biomedical model towards the more rights-based, recovery-oriented, person-centered, trauma-informed approach.
Globally, there is a call, a call that can’t be ignored for this shift. We really need to reconceptualise how we actually support people with mental health difficulties.
In Ireland, we need to update the Mental Health Act. I know Mental Health Reform has done great work on that, which I very much support, to be more in line with legislation on the United Nations Convention on the Rights of Persons with Disabilities (UNCRPD).”